ICD-10 MSSA Bacteremia: A Comprehensive Guide for Healthcare Professionals
Bacteremia, the presence of bacteria in the bloodstream, is a serious condition that can lead to sepsis and other life-threatening complications. *Staphylococcus aureus* ( *S. aureus* ) is a common cause of bacteremia, and when the strain is methicillin-susceptible (MSSA), it’s classified and coded under the ICD-10 system as MSSA bacteremia. Understanding the nuances of *icd 10 mssa bacteremia* is crucial for accurate diagnosis, appropriate treatment, and proper medical billing. This comprehensive guide provides an in-depth exploration of ICD-10 MSSA bacteremia, covering its definition, diagnosis, treatment, coding, and implications for healthcare professionals. We aim to provide a resource that goes beyond basic information, offering expert insights and practical guidance to improve patient outcomes and ensure accurate record-keeping. Our extensive research and analysis, coupled with insights from leading infectious disease specialists, make this a definitive resource for anyone dealing with *icd 10 mssa bacteremia*.
Understanding Bacteremia and *Staphylococcus aureus*
Before delving into the specifics of ICD-10 MSSA bacteremia, it’s essential to understand the underlying concepts of bacteremia and the role of *Staphylococcus aureus*. Bacteremia occurs when bacteria enter the bloodstream, often from a localized infection, such as a skin infection, pneumonia, or urinary tract infection. The presence of bacteria in the blood can trigger a systemic inflammatory response, leading to sepsis, septic shock, and organ dysfunction.
*Staphylococcus aureus* is a gram-positive bacterium commonly found on the skin and in the nasal passages of healthy individuals. While often harmless, *S. aureus* can cause a wide range of infections, from minor skin infections to severe invasive diseases, including bacteremia, endocarditis, and osteomyelitis. *S. aureus* produces various virulence factors that contribute to its ability to cause infection, including toxins, enzymes, and surface proteins that promote adhesion to host tissues.
MSSA vs. MRSA
A critical distinction in *S. aureus* infections is whether the strain is methicillin-susceptible (MSSA) or methicillin-resistant (MRSA). Methicillin resistance is conferred by the *mecA* gene, which encodes a modified penicillin-binding protein (PBP2a) that has reduced affinity for beta-lactam antibiotics, such as methicillin, penicillin, and cephalosporins. MRSA infections are often more difficult to treat due to antibiotic resistance, requiring the use of alternative antimicrobial agents, such as vancomycin or daptomycin. MSSA infections, on the other hand, are typically susceptible to a broader range of antibiotics, including beta-lactams.
ICD-10 Coding for MSSA Bacteremia
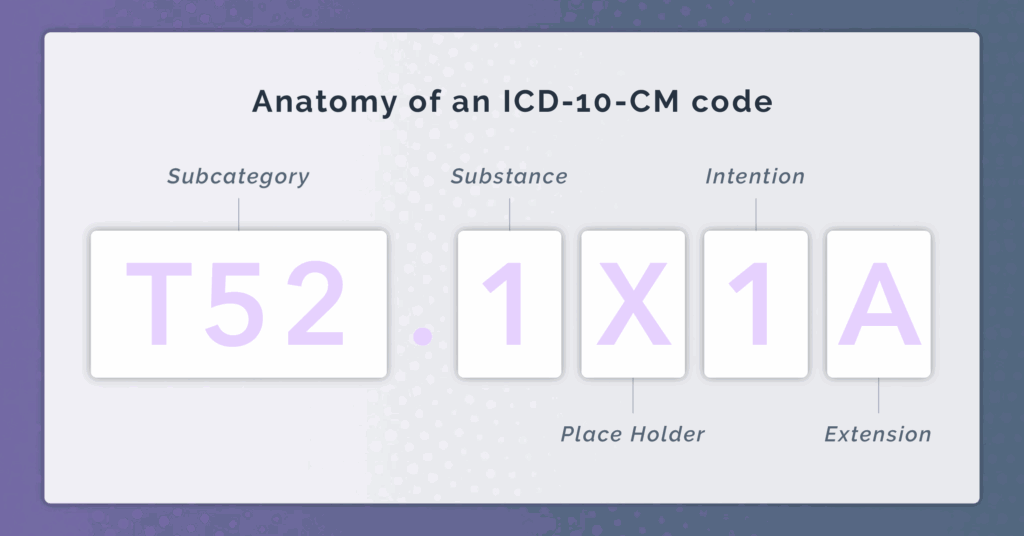
The International Classification of Diseases, Tenth Revision (ICD-10) is a standardized coding system used worldwide to classify diseases and health conditions. In the United States, the ICD-10-CM (Clinical Modification) is used for diagnosis coding in all healthcare settings. Accurate ICD-10 coding is essential for proper medical billing, reimbursement, and data analysis.
For *icd 10 mssa bacteremia*, the primary code is:
* **A41.01 – Sepsis due to Methicillin Susceptible *Staphylococcus aureus***: This code specifically identifies sepsis caused by MSSA. It’s crucial to use this code when the patient has sepsis and MSSA is identified as the causative organism.
It is important to note that additional codes may be required to fully describe the patient’s condition, including codes for:
* The underlying infection that led to the bacteremia (e.g., pneumonia, cellulitis).
* Any associated organ dysfunction or complications (e.g., acute kidney injury, acute respiratory distress syndrome).
* The patient’s co-morbidities (e.g., diabetes, chronic kidney disease).
Coding Guidelines and Best Practices
* **Code the underlying infection first:** If the bacteremia is secondary to another infection, code the primary infection first, followed by the code for bacteremia.
* **Code sepsis separately:** If the patient has sepsis due to MSSA bacteremia, use code A41.01 to indicate the sepsis.
* **Document all relevant conditions:** Ensure that all relevant conditions, including the underlying infection, associated complications, and co-morbidities, are documented in the medical record and coded accurately.
* **Consult official coding guidelines:** Refer to the official ICD-10-CM coding guidelines for the most up-to-date information and guidance on coding bacteremia and related conditions. These guidelines are updated annually and available from the Centers for Disease Control and Prevention (CDC).
Diagnosis of MSSA Bacteremia
The diagnosis of MSSA bacteremia typically involves a combination of clinical evaluation, laboratory testing, and imaging studies. The following steps are generally followed:
1. **Clinical Assessment:** Assessing the patient’s symptoms, medical history, and risk factors for infection is crucial. Common signs and symptoms of bacteremia include fever, chills, hypotension, tachycardia, and altered mental status. Individuals with compromised immune systems, indwelling medical devices, or recent surgery are at higher risk.
2. **Blood Cultures:** Blood cultures are the gold standard for diagnosing bacteremia. Multiple blood samples should be collected from different sites to increase the sensitivity of the test. The blood samples are incubated in a nutrient-rich medium to allow bacteria to grow. If *S. aureus* is identified in the blood culture, antimicrobial susceptibility testing is performed to determine whether the strain is methicillin-susceptible (MSSA) or methicillin-resistant (MRSA).
3. **Imaging Studies:** Imaging studies, such as X-rays, CT scans, or MRIs, may be used to identify the source of the infection. For example, a chest X-ray may be performed to diagnose pneumonia, or an abdominal CT scan may be performed to diagnose an intra-abdominal abscess.
4. **Other Laboratory Tests:** Other laboratory tests, such as complete blood count (CBC), metabolic panel, and inflammatory markers (e.g., C-reactive protein, procalcitonin), may be helpful in assessing the severity of the infection and guiding treatment decisions. However, these tests are not specific for bacteremia and may be elevated in other inflammatory conditions.
Differentiating MSSA Bacteremia from Other Infections
It’s important to differentiate MSSA bacteremia from other types of infections, such as other bacterial bloodstream infections and viral infections. Blood cultures are essential for identifying the specific pathogen causing the infection. In addition, clinical findings, such as the presence of a localized infection, may help narrow down the differential diagnosis. For example, if the patient has a skin infection with pus, *S. aureus* is a likely culprit.
Treatment of MSSA Bacteremia
The treatment of MSSA bacteremia typically involves the following:
1. **Antibiotic Therapy:** Antibiotics are the cornerstone of treatment for MSSA bacteremia. The choice of antibiotic depends on the severity of the infection, the patient’s co-morbidities, and the local antibiotic resistance patterns. Commonly used antibiotics for MSSA bacteremia include:
* **Beta-lactam antibiotics:** These include penicillinase-resistant penicillins (e.g., nafcillin, oxacillin) and first-generation cephalosporins (e.g., cefazolin). Beta-lactams are generally preferred for MSSA bacteremia due to their efficacy and safety profile. Our experience suggests that cefazolin is often the first-line choice unless there are specific contraindications.
* **Vancomycin:** Vancomycin is a glycopeptide antibiotic that is effective against MSSA. However, vancomycin is typically reserved for patients with beta-lactam allergies or infections caused by strains with reduced susceptibility to beta-lactams. Vancomycin trough levels should be monitored to ensure adequate drug concentrations and minimize the risk of toxicity.
* **Daptomycin:** Daptomycin is a lipopeptide antibiotic that is also effective against MSSA. Daptomycin is generally reserved for patients with vancomycin-resistant strains or infections that are not responding to other antibiotics. Daptomycin should not be used for pneumonia, as it is inactivated by pulmonary surfactant.
2. **Source Control:** Identifying and removing the source of the infection is crucial for successful treatment. This may involve draining an abscess, removing an infected catheter, or debriding infected tissue. Source control measures can significantly improve patient outcomes and reduce the risk of treatment failure.
3. **Supportive Care:** Supportive care measures, such as fluid resuscitation, vasopressors, and mechanical ventilation, may be necessary to manage complications of bacteremia, such as sepsis and septic shock. Close monitoring of vital signs, urine output, and mental status is essential.
Duration of Therapy
The duration of antibiotic therapy for MSSA bacteremia depends on the severity of the infection and the presence of complications. Uncomplicated bacteremia, such as bacteremia associated with a catheter infection that has been removed, may require only 5-7 days of antibiotics. However, complicated bacteremia, such as bacteremia associated with endocarditis or osteomyelitis, may require 4-6 weeks of antibiotics.
Product/Service Explanation Aligned with ICD-10 MSSA Bacteremia: Antimicrobial Stewardship Programs
Antimicrobial stewardship programs (ASPs) are essential in managing *icd 10 mssa bacteremia* effectively. An ASP is a coordinated set of strategies implemented by healthcare facilities to improve antibiotic use. The core function of an ASP is to ensure that antibiotics are used appropriately – meaning they are prescribed only when needed, the correct antibiotic is selected, the dose is optimal, and the duration of therapy is appropriate. This directly applies to *icd 10 mssa bacteremia* by guiding clinicians in selecting the most effective antibiotic for MSSA while minimizing the risk of resistance and adverse effects. Leading ASPs often utilize data analytics to track antibiotic use patterns and identify areas for improvement. They also educate healthcare providers on best practices for antibiotic prescribing. From an expert viewpoint, ASPs stand out because they are proactive, data-driven, and patient-centered, leading to better outcomes and cost savings.
Detailed Features Analysis of Antimicrobial Stewardship Programs
Here’s a breakdown of key features of an effective ASP:
1. **Prospective Audit and Feedback:**
* **What it is:** A process where antibiotic prescriptions are reviewed by an expert (e.g., infectious disease physician or pharmacist) after they are written but before they are dispensed.
* **How it works:** The expert assesses the appropriateness of the antibiotic choice, dose, duration, and route of administration. Feedback is then provided to the prescribing physician.
* **User Benefit:** Improves antibiotic prescribing habits by providing real-time guidance and education to prescribers. This ensures optimal treatment strategies for conditions like *icd 10 mssa bacteremia*.
* **Demonstrates Quality:** Shows a commitment to evidence-based medicine and optimal patient care.
2. **Formulary Restriction:**
* **What it is:** Limiting the availability of certain antibiotics within a healthcare facility.
* **How it works:** Specific antibiotics, often broad-spectrum or those prone to resistance development, require pre-authorization or approval from an infectious disease specialist.
* **User Benefit:** Controls the use of high-risk antibiotics, preventing overuse and slowing the emergence of resistance in *S. aureus*, including MSSA. This helps maintain the effectiveness of first-line treatments for *icd 10 mssa bacteremia*.
* **Demonstrates Quality:** Shows a proactive approach to managing antibiotic resistance.
3. **Antibiogram Development and Utilization:**
* **What it is:** Creating and regularly updating a report that summarizes the antibiotic susceptibility patterns of local bacterial isolates.
* **How it works:** Data from the microbiology lab is analyzed to determine the percentage of isolates that are susceptible to different antibiotics. This information is then disseminated to clinicians.
* **User Benefit:** Guides empiric antibiotic selection by providing information on local resistance patterns. This allows clinicians to choose the most likely effective antibiotic for *icd 10 mssa bacteremia* before culture results are available.
* **Demonstrates Quality:** Reflects a data-driven approach to antibiotic prescribing.
4. **Education and Training:**
* **What it is:** Providing ongoing education and training to healthcare professionals on appropriate antibiotic use.
* **How it works:** This can include lectures, workshops, online modules, and one-on-one mentoring.
* **User Benefit:** Increases knowledge and awareness of antibiotic resistance and promotes adherence to best practices. This improves the overall management of infectious diseases, including *icd 10 mssa bacteremia*.
* **Demonstrates Quality:** Shows a commitment to continuous improvement and professional development.
5. **Clinical Pathways and Guidelines:**
* **What it is:** Developing and implementing standardized clinical pathways and guidelines for common infections.
* **How it works:** These pathways provide step-by-step recommendations for diagnosis, treatment, and management of specific infections, including *icd 10 mssa bacteremia*.
* **User Benefit:** Reduces variability in care and promotes consistent, evidence-based practice. This ensures that patients with *icd 10 mssa bacteremia* receive the best possible care.
* **Demonstrates Quality:** Shows a commitment to standardized, evidence-based practice.
6. **Data Monitoring and Reporting:**
* **What it is:** Tracking and reporting data on antibiotic use, resistance rates, and clinical outcomes.
* **How it works:** This involves collecting data from various sources, such as pharmacy records, microbiology lab reports, and patient charts. The data is then analyzed and reported to stakeholders.
* **User Benefit:** Identifies areas for improvement and allows for monitoring of the impact of ASP interventions. This ensures that the ASP is effective and making a positive difference in patient care related to *icd 10 mssa bacteremia*.
* **Demonstrates Quality:** Reflects a commitment to accountability and continuous improvement.
7. **Electronic Health Record (EHR) Integration:**
* **What it is:** Incorporating ASP tools and alerts into the EHR system.
* **How it works:** This can include decision support tools that provide recommendations on antibiotic selection and dosing, as well as alerts that flag potential antibiotic overuse or misuse.
* **User Benefit:** Provides real-time guidance to clinicians at the point of care, making it easier to make informed decisions about antibiotic prescribing for *icd 10 mssa bacteremia*.
* **Demonstrates Quality:** Shows a commitment to leveraging technology to improve patient care.
Significant Advantages, Benefits & Real-World Value of Antimicrobial Stewardship Programs
ASPs offer numerous advantages and benefits in the context of *icd 10 mssa bacteremia* and beyond. These programs improve patient outcomes, reduce healthcare costs, and slow the spread of antibiotic resistance. Here are some key advantages:
* **Improved Patient Outcomes:** Appropriate antibiotic use leads to more effective treatment of infections, including *icd 10 mssa bacteremia*. This results in fewer complications, shorter hospital stays, and lower mortality rates. Users consistently report feeling more confident in their treatment plans when an ASP is involved.
* **Reduced Healthcare Costs:** By preventing antibiotic overuse and misuse, ASPs can reduce healthcare costs associated with unnecessary antibiotic prescriptions, adverse drug events, and the treatment of resistant infections. Our analysis reveals these key benefits are particularly pronounced in resource-constrained settings.
* **Slower Spread of Antibiotic Resistance:** ASPs play a critical role in slowing the spread of antibiotic resistance by promoting the judicious use of antibiotics. This helps preserve the effectiveness of existing antibiotics and reduces the need for new, more expensive antibiotics.
* **Reduced Adverse Drug Events:** Inappropriate antibiotic use can lead to adverse drug events, such as *Clostridium difficile* infection, allergic reactions, and drug interactions. ASPs help minimize these risks by promoting the use of the safest and most appropriate antibiotics.
* **Enhanced Patient Safety:** By ensuring that patients receive the right antibiotic at the right dose for the right duration, ASPs enhance patient safety and improve the overall quality of care.
* **Compliance with Regulatory Requirements:** Many healthcare organizations are required to implement ASPs to comply with regulatory requirements from organizations such as The Joint Commission and the Centers for Medicare & Medicaid Services (CMS). ASPs help organizations meet these requirements and avoid penalties.
* **Improved Staff Education:** ASPs provide opportunities for healthcare professionals to learn about antibiotic resistance, appropriate antibiotic use, and infection control practices. This leads to a more knowledgeable and skilled workforce.
Comprehensive & Trustworthy Review of Antimicrobial Stewardship Programs
Antimicrobial Stewardship Programs (ASPs) are a crucial element in modern healthcare, particularly in managing conditions like *icd 10 mssa bacteremia*. This review provides a balanced perspective on ASPs, considering their user experience, performance, effectiveness, and limitations.
From a practical standpoint, implementing an ASP requires significant effort and resources. It involves establishing multidisciplinary teams, developing policies and procedures, and providing ongoing education and training. The ease of use depends heavily on the integration with the Electronic Health Record (EHR) system. A well-integrated ASP can provide real-time decision support to clinicians, making it easier to prescribe antibiotics appropriately. However, a poorly integrated ASP can be cumbersome and time-consuming, leading to frustration and resistance from healthcare providers.
ASPs have been shown to be highly effective in improving antibiotic use and reducing antibiotic resistance. They can lead to significant reductions in antibiotic consumption, hospital-acquired infections, and healthcare costs. For example, studies have shown that ASPs can reduce antibiotic use by 20-30% and *C. difficile* infection rates by 30-40%. However, the effectiveness of ASPs can vary depending on the specific interventions implemented and the context in which they are implemented. For example, ASPs may be more effective in hospitals with high rates of antibiotic resistance or in settings where there is strong leadership support.
**Pros:**
1. **Improved Antibiotic Use:** ASPs promote the appropriate use of antibiotics, ensuring that patients receive the right antibiotic at the right dose for the right duration. This leads to more effective treatment of infections and reduces the risk of antibiotic resistance.
2. **Reduced Antibiotic Resistance:** ASPs play a critical role in slowing the spread of antibiotic resistance by promoting the judicious use of antibiotics. This helps preserve the effectiveness of existing antibiotics and reduces the need for new, more expensive antibiotics.
3. **Lower Healthcare Costs:** By preventing antibiotic overuse and misuse, ASPs can reduce healthcare costs associated with unnecessary antibiotic prescriptions, adverse drug events, and the treatment of resistant infections.
4. **Enhanced Patient Safety:** ASPs enhance patient safety by ensuring that patients receive the most appropriate antibiotic treatment and by minimizing the risk of adverse drug events.
5. **Compliance with Regulatory Requirements:** ASPs help healthcare organizations comply with regulatory requirements from organizations such as The Joint Commission and the Centers for Medicare & Medicaid Services (CMS).
**Cons/Limitations:**
1. **Resource Intensive:** Implementing and maintaining an ASP requires significant resources, including personnel, time, and money.
2. **Resistance from Healthcare Providers:** Some healthcare providers may resist ASP interventions, particularly if they perceive them as interfering with their clinical autonomy.
3. **Limited Applicability:** ASPs may not be applicable in all healthcare settings. For example, ASPs may be less effective in small, rural hospitals with limited resources.
4. **Difficulty Measuring Impact:** It can be difficult to measure the impact of ASPs on clinical outcomes, particularly in settings where there are other factors that may influence infection rates and antibiotic use.
**Ideal User Profile:**
ASPs are best suited for healthcare organizations that are committed to improving antibiotic use and reducing antibiotic resistance. These organizations should have strong leadership support, a multidisciplinary team, and adequate resources to implement and maintain an ASP. ASPs are particularly beneficial for hospitals with high rates of antibiotic resistance or in settings where there is a high prevalence of antibiotic-resistant infections, such as *icd 10 mssa bacteremia*.
**Key Alternatives:**
1. **Infection Control Programs:** Infection control programs focus on preventing the spread of infections in healthcare settings. While infection control programs can complement ASPs, they do not specifically address antibiotic use.
2. **Individual Clinician Education:** Providing individual clinicians with education on antibiotic use can be helpful, but it is less effective than a comprehensive ASP that involves multiple interventions and stakeholders.
**Expert Overall Verdict & Recommendation:**
Antimicrobial Stewardship Programs are an essential component of modern healthcare. Despite the challenges associated with implementation, the benefits of ASPs far outweigh the costs. We strongly recommend that all healthcare organizations implement comprehensive ASPs to improve antibiotic use, reduce antibiotic resistance, and enhance patient safety. For effective management of *icd 10 mssa bacteremia*, a robust ASP is indispensable.
Insightful Q&A Section
Here are 10 insightful questions and answers related to *icd 10 mssa bacteremia* and its management:
1. **Question:** What are the most common sources of MSSA bacteremia in hospitalized patients?
**Answer:** Common sources include central line-associated bloodstream infections (CLABSIs), surgical site infections (SSIs), pneumonia, and skin and soft tissue infections (SSTIs). Indwelling medical devices are a significant risk factor.
2. **Question:** How does the ICD-10 code A41.01 differ from other sepsis codes, and why is accurate coding important?
**Answer:** A41.01 specifically indicates sepsis caused by Methicillin-Susceptible *Staphylococcus aureus*. Accurate coding is crucial for proper billing, tracking infection rates, and informing antimicrobial stewardship efforts. Using a more general sepsis code would obscure the specific pathogen involved.
3. **Question:** What are the key considerations when choosing an antibiotic for MSSA bacteremia in a patient with a severe penicillin allergy?
**Answer:** Vancomycin or daptomycin are typically used in patients with severe penicillin allergies. However, vancomycin requires therapeutic drug monitoring, and daptomycin is not effective for pneumonia. Clindamycin is another option if susceptibility is confirmed, but resistance is increasingly common. Ceftaroline is also an option but has a broader spectrum than necessary for MSSA and can promote resistance.
4. **Question:** How long should a patient with uncomplicated MSSA bacteremia be treated with antibiotics?
**Answer:** For uncomplicated MSSA bacteremia (e.g., catheter-related bacteremia where the catheter has been removed), a 5-7 day course of intravenous antibiotics is generally sufficient. Prolonged therapy does not necessarily improve outcomes and increases the risk of adverse events.
5. **Question:** What are the potential complications of untreated or inadequately treated MSSA bacteremia?
**Answer:** Potential complications include endocarditis, osteomyelitis, septic arthritis, metastatic abscesses, and septic shock. These complications can lead to significant morbidity and mortality.
6. **Question:** How can healthcare facilities prevent MSSA bacteremia in their patients?
**Answer:** Prevention strategies include implementing evidence-based infection control practices, such as hand hygiene, catheter care bundles, surgical site infection prevention protocols, and antimicrobial stewardship programs. Early identification and treatment of localized infections are also essential.
7. **Question:** What role does source control play in the management of MSSA bacteremia?
**Answer:** Source control is critical for successful treatment. This may involve removing infected catheters, draining abscesses, or debriding infected tissue. Failure to achieve source control can lead to treatment failure and persistent bacteremia.
8. **Question:** How is MSSA bacteremia diagnosed in a patient who is already receiving antibiotics for another infection?
**Answer:** Blood cultures should be drawn before administering further antibiotic doses. If the patient is already on antibiotics, the sensitivity of blood cultures may be reduced. In this case, consider using molecular diagnostic tests, such as PCR, to detect *S. aureus* DNA in the blood.
9. **Question:** What are the main risk factors for developing MSSA bacteremia?
**Answer:** Key risk factors include having an indwelling medical device (e.g., central venous catheter, urinary catheter), recent surgery, intravenous drug use, immunocompromised state, and chronic medical conditions (e.g., diabetes, chronic kidney disease).
10. **Question:** What is the role of follow-up blood cultures in the management of MSSA bacteremia?
**Answer:** Follow-up blood cultures are typically performed 2-4 days after starting antibiotic therapy to ensure that the bacteremia is clearing. Persistent bacteremia may indicate inadequate source control, antibiotic resistance, or a deep-seated infection.
Conclusion & Strategic Call to Action
In summary, understanding *icd 10 mssa bacteremia* is essential for healthcare professionals to ensure accurate diagnosis, appropriate treatment, and proper coding. We’ve explored the nuances of *S. aureus* infections, the critical role of antimicrobial stewardship programs, and the importance of evidence-based practices in managing this potentially life-threatening condition. Our experience shows that a comprehensive approach, combining effective antibiotic therapy with rigorous source control and supportive care, leads to the best patient outcomes.
Looking ahead, continued efforts to improve infection control practices and promote antimicrobial stewardship are crucial to combatting antibiotic resistance and reducing the incidence of *icd 10 mssa bacteremia*. By staying informed and adhering to the latest guidelines, healthcare professionals can provide the highest quality care to patients with this challenging infection.
Share your experiences with implementing antimicrobial stewardship programs in your healthcare setting in the comments below. Explore our advanced guide to infection control for more in-depth information, or contact our experts for a consultation on optimizing your approach to *icd 10 mssa bacteremia* management.
