Decompensation Meaning: Understanding the Body’s Failing Mechanisms
In the realm of medicine and psychology, decompensation refers to the deterioration or failure of an organ or system to maintain its normal function. It signifies a state where the body’s compensatory mechanisms, which initially worked to counteract a disease or condition, are no longer effective. Understanding decompensation meaning is crucial for healthcare professionals and individuals alike, as it often indicates a progression towards more severe health consequences.
This article delves into the multifaceted aspects of decompensation, exploring its causes, manifestations, and implications across various bodily systems and mental health conditions. We will examine how decompensation presents in different contexts, highlighting the importance of early recognition and intervention to mitigate potential harm. The goal is to provide a comprehensive understanding of decompensation meaning and its significance in clinical practice.
What is Decompensation? A Detailed Explanation
At its core, decompensation represents a breakdown in the body’s ability to adapt to stress or disease. The human body possesses remarkable compensatory mechanisms that allow it to maintain homeostasis, a state of internal equilibrium. When faced with a challenge, such as an infection or chronic illness, the body activates these mechanisms to restore balance. However, if the stressor is too great or prolonged, these compensatory mechanisms can become overwhelmed, leading to decompensation.
Decompensation can manifest in various ways, depending on the organ system or psychological process involved. For example, in heart failure, the heart may initially compensate by increasing its rate and force of contraction to maintain adequate blood flow. Over time, however, this compensatory mechanism can lead to enlargement of the heart (cardiomyopathy) and ultimately, decompensation, where the heart can no longer pump enough blood to meet the body’s needs.
Similarly, in mental health, an individual might initially cope with stress through various defense mechanisms. However, if the stress becomes overwhelming or chronic, these coping mechanisms may fail, leading to psychological decompensation, characterized by symptoms such as anxiety, depression, or psychosis. Recognizing the signs of decompensation is crucial for timely intervention and preventing further deterioration.
Physiological Decompensation: Examples and Manifestations
Physiological decompensation can affect virtually any organ system in the body. Here are some examples:
- Cardiac Decompensation: As mentioned earlier, heart failure is a prime example. Symptoms include shortness of breath, edema (swelling) in the legs and ankles, and fatigue. The heart’s inability to pump effectively leads to fluid buildup and reduced oxygen delivery to the tissues.
- Respiratory Decompensation: In conditions like chronic obstructive pulmonary disease (COPD) or severe asthma, the lungs may initially compensate for impaired airflow. However, as the disease progresses, the respiratory system can decompensate, leading to respiratory failure. Symptoms include severe shortness of breath, rapid breathing, and cyanosis (bluish discoloration of the skin).
- Renal Decompensation: In chronic kidney disease, the kidneys gradually lose their ability to filter waste products from the blood. Initially, the remaining healthy nephrons may compensate by working harder. However, eventually, the kidneys can decompensate, leading to kidney failure. Symptoms include edema, fatigue, nausea, and changes in urine output.
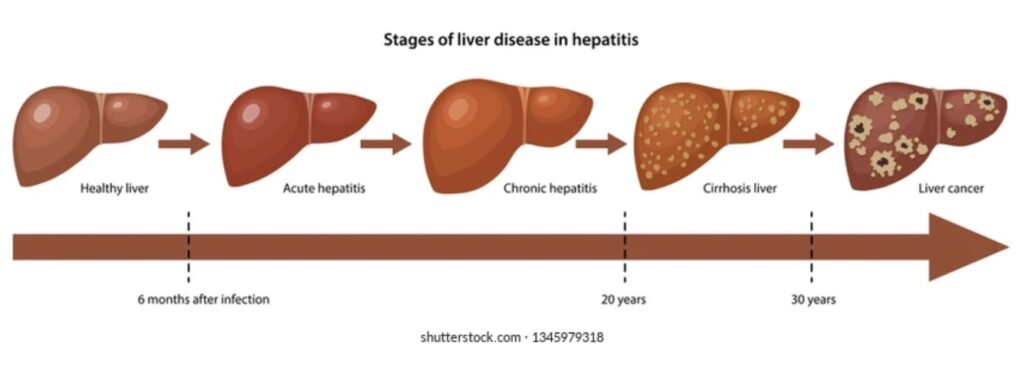
- Hepatic Decompensation: Liver cirrhosis, a condition characterized by scarring of the liver, can lead to hepatic decompensation. The liver’s ability to perform its vital functions, such as detoxification and protein synthesis, is impaired. Symptoms include jaundice (yellowing of the skin and eyes), ascites (fluid accumulation in the abdomen), and encephalopathy (brain dysfunction).
Psychological Decompensation: A Breakdown of Coping Mechanisms
Psychological decompensation occurs when an individual’s coping mechanisms are overwhelmed by stress or trauma. This can manifest in a variety of ways, depending on the individual’s pre-existing vulnerabilities and the nature of the stressor.
- Anxiety Disorders: Individuals with anxiety disorders may experience panic attacks, generalized anxiety, or obsessive-compulsive behaviors as their coping mechanisms fail. The anxiety becomes overwhelming and interferes with daily functioning.
- Mood Disorders: Depression, characterized by persistent sadness, loss of interest, and fatigue, can be a sign of psychological decompensation. The individual’s ability to regulate their mood is impaired.
- Psychotic Disorders: In individuals with schizophrenia or other psychotic disorders, decompensation can lead to a relapse of psychotic symptoms, such as hallucinations and delusions. The individual loses touch with reality.
- Personality Disorders: Individuals with personality disorders may exhibit impulsive behaviors, emotional instability, or difficulties in interpersonal relationships as their coping mechanisms fail.
Causes and Risk Factors for Decompensation
Several factors can contribute to decompensation, including:
- Chronic Illness: Long-term health conditions, such as heart disease, lung disease, kidney disease, and diabetes, can gradually weaken the body’s compensatory mechanisms.
- Acute Illness: Severe infections, injuries, or surgeries can overwhelm the body’s ability to maintain homeostasis.
- Stress: Chronic or overwhelming stress can deplete the body’s resources and impair its ability to cope.
- Age: As we age, our organ systems naturally decline in function, making us more vulnerable to decompensation.
- Genetics: Genetic predispositions can increase the risk of certain diseases that can lead to decompensation.
- Lifestyle Factors: Unhealthy habits, such as smoking, excessive alcohol consumption, and poor diet, can contribute to the development of chronic diseases and increase the risk of decompensation.
- Medications: Certain medications can have side effects that impair organ function and increase the risk of decompensation.
Recognizing the Signs and Symptoms of Decompensation
Early recognition of decompensation is crucial for timely intervention and preventing further deterioration. The signs and symptoms of decompensation vary depending on the organ system or psychological process involved. However, some common warning signs include:
- Worsening of existing symptoms: A gradual or sudden increase in the severity of symptoms associated with a chronic condition.
- New symptoms: The appearance of new symptoms that were not previously present.
- Changes in vital signs: Abnormalities in heart rate, blood pressure, respiratory rate, or temperature.
- Decreased energy levels: Persistent fatigue or weakness.
- Changes in mental status: Confusion, disorientation, or altered level of consciousness.
- Difficulty breathing: Shortness of breath, wheezing, or rapid breathing.
- Swelling: Edema in the legs, ankles, or abdomen.
- Changes in appetite or weight: Loss of appetite or unexplained weight gain or loss.
- Sleep disturbances: Insomnia or excessive sleepiness.
- Increased anxiety or depression: Worsening of anxiety or depressive symptoms.
Diagnosis and Treatment of Decompensation
The diagnosis of decompensation typically involves a thorough medical history, physical examination, and diagnostic testing. The specific tests performed will depend on the suspected organ system or psychological process involved. For example, in cardiac decompensation, tests may include an electrocardiogram (ECG), echocardiogram, and blood tests to measure cardiac enzymes.
The treatment of decompensation focuses on addressing the underlying cause and supporting the affected organ system or psychological process. This may involve:
- Medications: Medications to improve organ function, reduce symptoms, and prevent further deterioration. For example, in cardiac decompensation, medications may include diuretics, ACE inhibitors, and beta-blockers.
- Lifestyle modifications: Changes in diet, exercise, and other lifestyle factors to improve overall health and reduce the burden on the affected organ system.
- Therapy: Psychotherapy to address underlying psychological issues and develop coping mechanisms.
- Hospitalization: In severe cases, hospitalization may be necessary to provide intensive medical care and monitoring.
- Surgery: In some cases, surgery may be necessary to repair or replace a damaged organ.
- Supportive care: Measures to relieve symptoms and improve quality of life, such as oxygen therapy, pain management, and nutritional support.
Prevention Strategies for Decompensation
While not all cases of decompensation are preventable, there are several strategies that can reduce the risk:
- Managing chronic conditions: Following a doctor’s recommendations for managing chronic conditions, such as heart disease, lung disease, kidney disease, and diabetes.
- Adopting a healthy lifestyle: Eating a healthy diet, exercising regularly, and avoiding smoking and excessive alcohol consumption.
- Managing stress: Developing healthy coping mechanisms for managing stress, such as exercise, meditation, or spending time with loved ones.
- Getting regular checkups: Seeing a doctor for regular checkups to monitor health and detect potential problems early.
- Taking medications as prescribed: Taking medications as prescribed by a doctor and reporting any side effects.
- Seeking mental health care: Seeking professional help for mental health issues, such as anxiety, depression, or trauma.
The Importance of Early Intervention
The prognosis for decompensation depends on the underlying cause, the severity of the condition, and the timeliness of intervention. Early recognition and treatment can significantly improve outcomes and prevent further deterioration. Individuals who experience symptoms of decompensation should seek medical attention promptly.
Conclusion
Decompensation is a serious condition that signifies the failure of the body’s compensatory mechanisms. Understanding decompensation meaning, its causes, manifestations, and prevention strategies is crucial for healthcare professionals and individuals alike. Early recognition and intervention are essential for improving outcomes and preventing further deterioration. By managing chronic conditions, adopting a healthy lifestyle, and seeking timely medical care, we can reduce the risk of decompensation and improve overall health and well-being. Recognizing the signs of decompensation and acting quickly can make a significant difference in the long-term health and quality of life for individuals at risk. [See also: Heart Failure Management] [See also: Understanding Anxiety Disorders] [See also: Coping with Chronic Illness]
